Angiolymphoid Hyperplasia with Eosinophilia of the Skin of the Scrotum and Penis
Abstract:
Angiolymphoid hyperplasia with eosinophilia is usually characterized clinically by solitary or multiple erytematous, dome-shaped dermal papules or nodules in the skin that may be eroded and occasionally associated with pain or pruritus. Most are located on the skin of the head and neck with predilection for the periauricular area. It may involve deep soft tissue and vessels as well as cases with visceral involvement [5, 9] and peripheral blood eosinophilia in 6% to 34% of patients [3]. Herein we report of a male patient presenting the disease in the skin of the penis and scrotum, a very rare location of this lesion.
Clinical History:
A 24-year old male presented to the outpatient clinic complaining of multiple, erythematous, elevated papules in the skin of the penis and scrotum, sometimes associated with pruritus and of several months duration [fig. 1].
Images:
-
Fig. 1: Confluent erythematous dome-shaped papules.
-
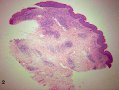
Fig. 2: Entire biopsy section shows aggregate nodules in the upper and mid-dermis.
-
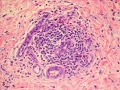
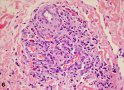
Fig. 3: Prominent capillary vessels and venules with lymphocytes and eosinophills (HE X400).
-
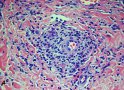
Fig. 4: Perivascular lymphoid infiltration with fibrosis (HE X 400).
-
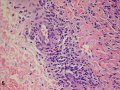
Fig. 5: Tombstone arrangement and hobnail pattern of endothelial cells (HE x 400).
-
Fig. 6: Heavy infiltration of eosinophils (HE x 400).
-
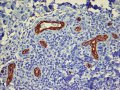
Fig. 7: Thick-walled vessels with non-canalized endothelial cells (white arrows) are evident with CD34 immunohistochemical stain (original magnification 400 X).
Macro and Microscopic Description:
A biopsy was taken of an entire papule. In the superficial and mid dermis, there are separate nodules [fig. 2]. Characteristic histologic features were present, including proliferation of thick-walled vessels, lined by prominent endothelial cells with a hobnail and “tombstone” appearance. A marked perivascular and interstitial infiltration of lymphocytes and numerous eosinophils are seen. Mild fibrosis in the dermis was also present [figs. 3, 4, 5, 6]. The immunohistochemical staining for CD 34 shows a prominent capillary pattern [fig.7].
Diagnosis:
Angiolymphoid Hyperplasia with Eosinophilia of the Skin of the Scrotum and Penis
Discussion:
This entity was first described in 1969 by Wells and Whimster [1] as “subcutaneous angiolymphoid hyperplasia with eosinophilia”. Wilson-Jones and Beehen [2] in the same year described similar lesions under the name of “inflammatory angiomatous nodules or pseudo, atypical pyogenic granuloma. The lesions are characterized clinically by solitary or multiple erythematous, dome-shaped dermal papules or nodules that may be eroded or crusted and associated occasionally with pain or pruritus. They average in size from 2 to 3 centimeters in diameter and are principally located in the skin of the head and neck with a special predilection for the periauricular area. It tends to occur in young adults between 20 and 40 years of age with a mean age of onset of 30 to 33 years. It is more common in women than in men. Peripheral blood eosinophilia ranging from 6% to 34% is present in about 20% of patients [3]. A history of trauma is found in some patients.
Most of the lesions are located intradermally or subcutaneous but may involve deep soft tissues and vessels. Besides the skin, this tumor has also been described in other tissues including large vessels, bone and heart [5], the oral cavity [7], the orbit [8], the lung [9], the breast [10] and the vulva [11, 12]. Only three cases has been reported to affect the skin of the penis [13, 14, 15], and the deep soft tissue of the corpus cavernosum [16].
Another terminology used to describe this process includes intravenous atypical vascular proliferation [4] and histiocytoid hemangioma [5]. In 1983 Enzinger and Weiss suggested the term “epithelioid hemangioma” for this vascular formation [6].
Histologically, this entity is characterized by both, a vascular and an inflammatory component. The vascular component is due to proliferation of small-sized capillaries and branching venules arranged in a lobular pattern. The vessels are lined by enlarged, prominent endothelial cells with a hobnail and a tombstone-like arrangement, as well as aggregates of non canalized endothelial cells.
The inflammatory component is composed of lymphocytes, abundant eosinophils and, in less quantity, plasma cells and mast cells. Angiolymphoid hyperplasia should be distinguished from Kimura´s disease [17, 18]. This disease is more common in young asian men and presents clinically as large, deep, subcutaneous plaques in the periauricular and submandibular regions, associated with enlarged regional lymph nodes and in most cases there is involvement of the salivary glands. Peripheral blood eosinophilia and elevated levels of serum IgE are found in most cases. Histologic features include prominent lymphoid follicles and fibrosis with a less prominent capillary proliferation and aggregates of non-canalized endothelial cells.
Other lesions to consider in the differential diagnosis include benign and malignant vascular lesions, as well as various reactives conditions dominated by infiltration of lymphocytes and eosinophils If the clinical presentation of ALHE is consider with its typical microscopic features, then one can exclude other vascular lesions such as epithelioid hemangioendothelioma, Kaposi sarcoma, epitheliod cutaneous angiosarcoma, lobular capillary hemangioma, pyogenic granuloma, angiomatous lymphoid hamartoma, granuloma faciale, lymphocytic or pseudolymphomas due to insect bites, and the recently described cutaneous epithelioid angiomatous nodule [19], which bears a striking resemblance to angiolymphoid hyperplasia with eosinophilia. Although the relationship between this cutaneous epithelioid angiomatus nodule and angiolymphoid hyperplasia has been suggested [20]. Recently Sangueza et. al. [21] proposed a classification of cutaneous vascular tumors in which the angiomatous epithelioid vascular nodule is probably a variant of epithelioid hemangioma [AHE].
References:
- Wells GC, Whimster IW. Subcutaneous angiolymphoid hyperplasia with eosinophilia. Br J Dermatol 1969; 81:1-15
- Wilson Jones E, Bleehan SS. Inflammatory angiomatous nodules with abnormal blood vessels occurring about the ears and scalp (pseudo or atypical pyogenic granuloma). Br J Dermatol 1969; 81:804-816
- Olsen TJ, Helwig EB. Angiolymphoid hyperplasia with eosinophilia: A clinicopathologic, study of 116 patients. J Am Acad Dermatol 1985; 12:781-796
- Rosai J, Akerman LR. Intravenous atypical vascular proliferation: A cutaneous lesion simulating a malignant blood vessel tumor. Arch Dermatol 1974; 109: 714-717
- Rosai J, Gold J, Landy R. The histiocytoid hemangiomas: A unifying concept embracing several previously described entities of skin, soft tissue, large vessels, bone and heart. Hum Pathol 1979; 10:707-730
- Enzinger FM, Weiss SW. Soft tissue tumors. St Louis: CV Mosby; 2001, p: 856
- Suzuki H, Hatamochi A., et al: A case of angiolymphoid hyperplasia with eosinophilia of the upper lip. J Dermatol 2005; 32:991-995
- Mc Eachren T, Browestein S, Jordan D, Montpetit V, Font R. Epithelioid hemangioma of the orbit. Ophtalmology 2000; 107:806-810
- Moran CA, Suster S. Angiolymphoid hyperplasia with eosinophilia (Epithelioid Hemangioma) of the lung. Am J Clin Pathol 2005; 123:762-765
- Nair M, Aaron M, Sharma MC. Angiolymphoid hyperplasia with eosinophilia (Epithelioid Hemangioma) of the breast. Report of a case. Surg Today 2000;30:747-749
- Aguilar A, Ambrojo P, Requena L., et al: Angiolymphoid hyperplasia with eosinophilia limited to the vulva. Clin Exp Dermatol 1990; 15: 65-67
- Scurry J, Demerstein G, Brenan J. Angiolymphoid hyperplasia with eosinophilia of the vulva. Aust NZ Obstet Gynecol 1995; 35: 347-348
- Raghunothan NR, Spurlock BA. Angiolymphoid hyperplasia with eosinophilia. Report of a case with penile lesion. Cancer 1981; 47:944-949
- Srigley JR, Ayala AG., et al: Epithelioid Hemangioma of the penis. A rare and distinctive vascular lesion. Arch Pathol Lab Med 1985; 109:51-54
- Villanueva Peña A, Rodríguez D., et al: Consideraciones en torno a la Hiperplasia Angiolinfoide con Eosinofilia (ALHE). A propósito de un caso localizado en el pene. Actas Urol Esp 2005; 29:113-117
- Fetsch JF, Sisterhem IA, Miettinen M, Davis CJ. Epithelioid Hemangioma of the penis. A clinicopathologic an Immunohistochemical Analysis of 19 cases, With Special Reference To Exuberant Examples often Confused with Epithelioid Hemangioendothelioma and Epithelioid Angiosarcoma. Am J Surg Pathol 2004;28: 523-533
- Briggs PL. Kimura disease is not angiolymphoid hyperplasia with eosinophilia: Clinical and pathological correlation with literature review and definition of diagnostic criteria. An Bras Dermatol 2006; 2: 167-173
- Hong Ch, Lester D, Thompson R., et al. Kimura Disease. A Clinicopathologic Study of 21 cases. Am J Surg Pathol 2004; 28:505-513
- Brenn T, Fletcher CD. Cutaneous epithelioid angiomatous nodule: a distinct lesion in the morphologic spectrum of epithelioid vascular tumors. Am J Dermatopathol 2004; 26:14-21
- Zamecnik M. Relationship between cutaneous epithelioid angiomatous nodule and epithelioid hemangioma. Am J Dermatopathol 2004; 26:351-352
- Sangueza, OP, Walsh SN, Sheehan DJ, Orland, AF, Llombart B, Requena L. Cuteneous epithelioid angiomatous nodule: a case series and proposed classification. Am J Dermatopathol 2008,30:16-20
Author:
Dr. Juan José Segura Fonseca, Departamento de Patología, Hospital San Juan de Dios, San José, Costa Rica